You can protect your future family with preconception genetic testing
Knowledge is power when it comes to starting or growing your family. That’s why the team at Texas Fertility Center recommends that patients get preconception genetic testing before trying to conceive. This advice about carrier screening follows guidelines from the American College of Medical Genetics and the American College of Obstetricians and Gynecologists.
Our Austin fertility clinic offers genetic testing to everyone who is thinking about becoming pregnant. The goal of this testing is to identify whether either parent carries an inheritable genetic disease. If one or both parents are carriers, our fertility specialists can help them avoid passing the genetic illness to their future children.
Preconception genetic testing can identify carriers of genetic illnesses
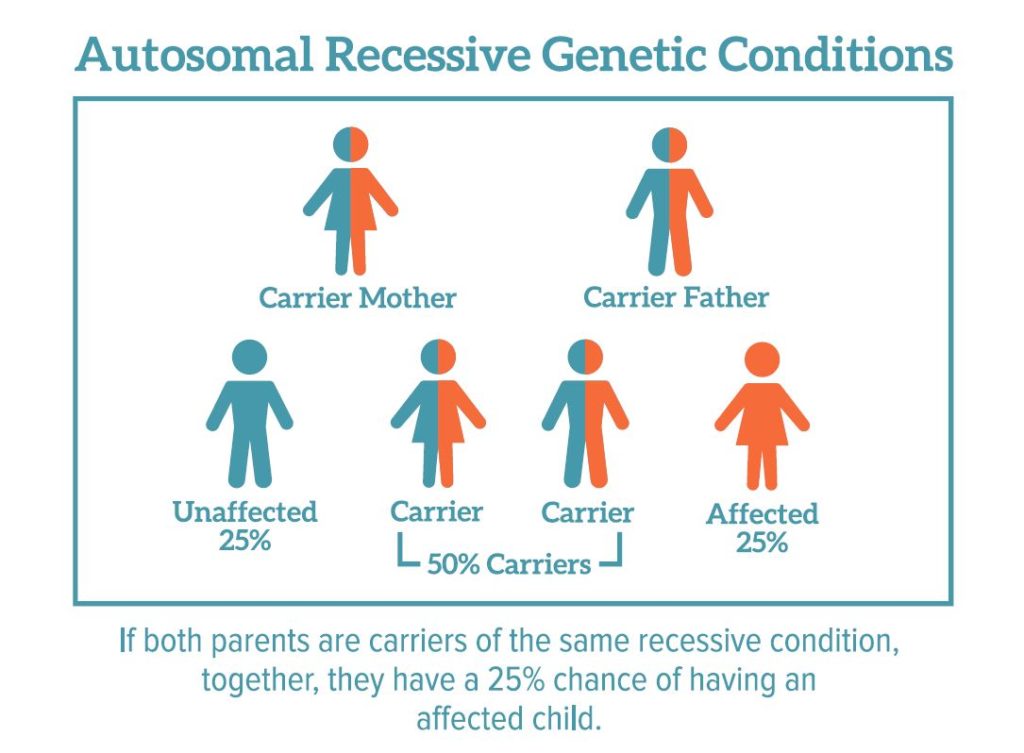
Carriers of genetic illnesses often don’t show signs of the disorder. However, if both parents are carriers of the same genetic mutation, their children are more likely to have the disease and experience symptoms.
The most common genetic disorders have an autosomal recessive mode of inheritance.
Without preconception genetic testing, parents may not realize that they are carriers who could pass a life-altering genetic disorder to their children. If carrier screening reveals that both parents carry a specific abnormal gene, there is hope. Fertility treatments like IVF and preimplantation genetic testing for monogenic disorders (PGT-M) can help them have a child without the genetic abnormality.
Exploring the types of preconception genetic testing
Because of advances in genetics, two types of genetic testing are available to men and women who visit our Austin fertility clinic. These two tests offer patients new hope for achieving their dream of having a healthy family.
One test requires a saliva sample from each parent. Laboratory professionals can screen a sample for more than 109 autosomal recessive genetic disorders. This saliva test can screen for many diseases and is relatively inexpensive.
The second test looks at pieces of genes from each parent. It requires a cheek swab or blood sample. This test can evaluate 200,000-300,000 small DNA fragments representing pieces of each known gene.
This second test can also evaluate the DNA from each IVF embryo. If an embryo is chromosomally abnormal, this test can determine whether the abnormality came from the egg or the sperm. This information can help patients who are considering donor eggs or donor sperm after facing recurrent miscarriage or repeated IVF failure.
If you would like to learn more about carrier screening at our Austin fertility clinic, please contact us today. You can rely on our caring and knowledgeable fertility doctors to help you welcome a healthy baby.