Learn more about the guidelines for transferring mosaic embryos
If you learn that some of your embryos have mosaicism, you might have questions about transferring mosaic embryos. We need additional research to fully understand the effect of mosaicism on embryo developmental potential. In the meantime, evidence-based results can guide you and your fertility care team in choosing the best embryos for transfer.
How does the report show mosaicism?
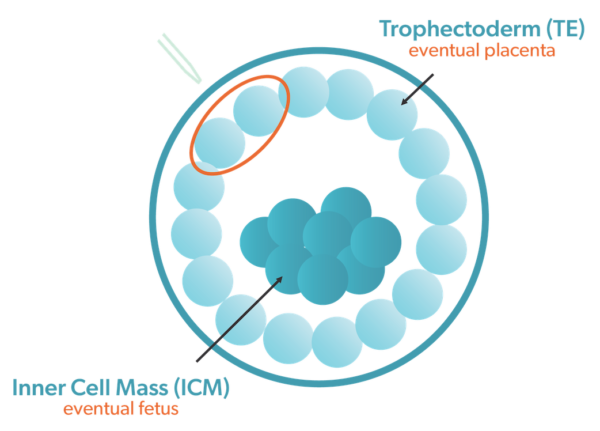 The biopsy of the trophectoderm layer, the group of cells that make up the placenta, goes to the reference lab for analysis. The PGT-A report shows whether each embryo is euploid (normal cell count) or aneuploid (abnormal cell count). The report then ranks each euploid embryo for the level of embryo mosaicism.
The biopsy of the trophectoderm layer, the group of cells that make up the placenta, goes to the reference lab for analysis. The PGT-A report shows whether each embryo is euploid (normal cell count) or aneuploid (abnormal cell count). The report then ranks each euploid embryo for the level of embryo mosaicism.
Mosaic embryo samples composed primarily of normal cells are classified as low-level mosaic (L-mos), and those that contain mostly abnormal cells are classified as high-level mosaic (H-mos).
Ovation® Genetics, a reference lab used by Texas Fertility Center, uses the following classification criteria for reporting mosaic embryo results.
- Normal (euploid) embryos contain 30% or fewer abnormal cells, whereas abnormal (aneuploid) embryos contain more than 70% abnormal cells.
- Low-level mosaic embryos contain 31% to 50% abnormal cells.
- High-level mosaic embryos contain 51% to 70% abnormal cells.
When a mosaic abnormality is identified in a biopsy sample, it is uncertain if abnormal cells will also be present throughout the rest of the embryo. For an embryo with a high level of mosaicism in the trophectoderm cells, there may be an increased likelihood that the ICM cells that form the embryo could also be abnormal (CoGEN, 2016 ).
Should you transfer a mosaic embryo?
An embryo that has a mosaic PGT-A result may have the potential to develop into either a chromosomally normal, abnormal or mosaic embryo. The effects of mosaicism depend on many factors, including where abnormal cells are located in the embryo and the proportion of cells that are abnormal. As such, the implications for each mosaic embryo can be difficult to predict.
Detecting mosaicism in embryos is an evolving science. Aneuploid embryos may contain some normal cells. Also, many euploid embryos may have a small percentage of mosaic abnormal cells that existing technology cannot reliably detect.
If your doctor recommends it, transferring mosaic embryos is possible. This is true if euploid embryos are not available, as healthy babies have been born from mosaic embryos. But if you are considering transferring a mosaic embryo, it is important to be aware of the risks.
Mosaic embryos are less likely to implant than euploid embryos and are more likely to result in miscarriage.
Mosaic embryos come with an increased risk of pregnancy complications or a child with a chromosome disorder.
In certain cases, we do not recommend transferring mosaic embryos. As such, it should be a last resort. Embryos with mosaic abnormalities involving multiple chromosomes have a very low likelihood for producing a successful pregnancy. There are also other findings that can indicate that transfer is not recommended.
- When mosaicism involves chromosomes 13, 14, 15, 18, 21, 22, X or Y, the risk increases for a child to be born with a chromosomal disorder.
- When mosaicism involves chromosomes 2, 7, or 16, there is an increased risk for severe pregnancy complications.
If you choose to transfer a mosaic embryo, we strongly recommend follow-up prenatal testing by amniocentesis.
Talk to your fertility specialist
Choosing to transfer a mosaic embryo is a decision that must be made with a thorough understanding of the potential implications and risks. Your fertility specialist can help you understand the implications and come to a decision that is right for you.













